Neuropathy symptoms can be effectively managed through lifestyle changes, such as a healthy diet, regular exercise, and medication, alongside addressing underlying conditions like diabetes.
Neuropathy vs radiculopathy: ever wondered how these two conditions differ? Both can cause discomfort, but understanding their nuances can lead to better management and relief. Let’s dive in!
Understanding neuropathy and radiculopathy
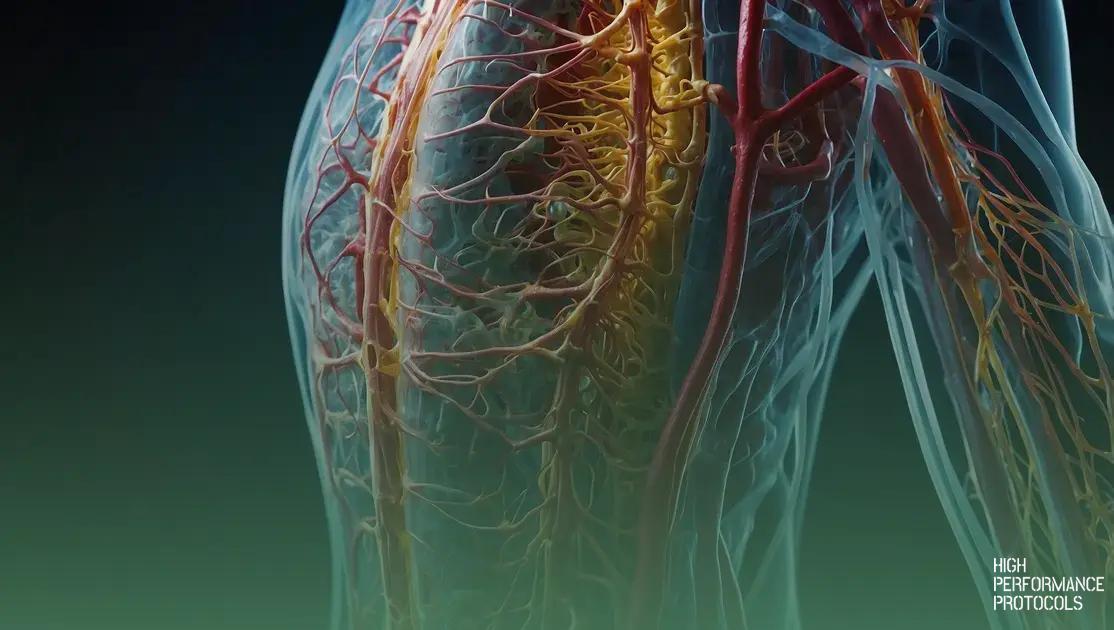
Neuropathy and radiculopathy are conditions that affect the nervous system, but they are different in nature. Neuropathy involves damage to the peripheral nerves, which can stem from various causes such as diabetes, infections, or injuries. This damage often leads to tingling sensations, muscle weakness, or pain in the affected areas.
On the other hand, radiculopathy occurs when there is compression or irritation of a nerve root in the spine, often due to herniated discs or spinal stenosis. This can radiate pain down the arms or legs, depending on which part of the spine is affected.
Symptoms of neuropathy typically include numbness, tingling, and pain, while radiculopathy often presents with pain that follows the path of a nerve, alongside muscle weakness and sensory loss. Understanding these differences is crucial for proper diagnosis and treatment.
For individuals experiencing these symptoms, it is important to seek medical advice for accurate diagnosis. Treatments may vary significantly between neuropathy and radiculopathy, requiring tailored approaches for effective relief.
Symptoms of neuropathy vs radiculopathy
When discussing neuropathy and radiculopathy, it is essential to recognize their distinct symptoms. Each condition presents unique challenges for those affected.
Neuropathy symptoms can vary widely, but common signs include:
- Tingling sensations in the hands or feet
- Numbness that can lead to a loss of feeling
- Muscle weakness in the affected areas
- Pain, which may be sharp or burning
- Extreme sensitivity to touch
These symptoms often indicate peripheral nerve damage, and they can be quite debilitating.
In contrast, radiculopathy tends to present symptoms that radiate along the nerve’s path:
- Severe pain that travels down the arm or leg
- Weakness in muscles served by the affected nerve
- Numbness in specific areas corresponding to the nerve root
- Reflex changes that may occur in the limbs
Understanding these differences is vital for diagnosis and treatment. If you are experiencing these symptoms, it’s important to consult with a healthcare professional for accurate evaluation.
Causes of peripheral nerve damage
Understanding the causes of peripheral nerve damage is crucial for diagnosis and treatment. Several factors can lead to the deterioration of peripheral nerves, impacting their ability to function properly.
One common cause is diabetes. Diabetic neuropathy arises when high blood sugar levels damage the nerves over time, leading to pain and loss of sensation.
Infections can also lead to nerve damage. Conditions such as Lyme disease, shingles, or HIV/AIDS can affect the peripheral nerves.
Physical injuries, including trauma from accidents or falls, can result in nerve compression or severing. Repetitive motion injuries from activities like typing can also contribute to nerve damage.
Other factors include toxic exposures, such as heavy metals or alcohol abuse, and nutritional deficiencies. Insufficient levels of vitamins like B12 can harm nerve health.
Understanding these causes is important because addressing them can prevent further damage and improve outcomes for those suffering from neuropathy.
Differentiating nerve conduction issues
Differentiating nerve conduction issues is essential for accurate diagnosis and treatment. Nerve conduction refers to the ability of nerves to transmit signals effectively. When these signals are disrupted, it can lead to various symptoms.
There are two primary types of nerve conduction issues: sensory nerve problems and motor nerve problems. Sensory nerve problems affect sensation and can lead to symptoms like numbness, tingling, or burning pain. Motor nerve issues impact muscle control, resulting in weakness or paralysis.
Common tests used to evaluate nerve conduction include nerve conduction studies (NCS) and electromyography (EMG). NCS measures how fast electrical impulses travel through the nerves, while EMG assesses the electrical activity of muscles.
Interpreting these tests can help distinguish between neuropathy, radiculopathy, and other nerve-related conditions. For instance, a slow nerve conduction speed might indicate peripheral nerve damage, while normal speeds can suggest a different issue.
Understanding these distinctions is vital for developing an appropriate treatment plan, which may include medications, physical therapy, or lifestyle changes.
Impact of diabetic neuropathy
The impact of diabetic neuropathy is significant and can affect various aspects of a person’s life. This condition arises from prolonged high blood sugar levels that damage the nerves, especially in the feet and hands.
Common symptoms include numbness, tingling, and sharp pain, which can make daily activities challenging. Many individuals experience difficulty walking, leading to a decreased quality of life.
Diabetic neuropathy can also increase the risk of foot injuries and infections. Due to reduced sensation, minor cuts or blisters may go unnoticed, leading to serious complications.
Additionally, this condition can profoundly affect mental health. Living with chronic pain and discomfort may result in anxiety or depression, further complicating management and self-care.
Managing diabetic neuropathy involves a combination of medication, lifestyle changes, and regular monitoring of blood sugar levels. It’s essential to work with healthcare providers to create a personalized management plan.
Chronic pain syndrome explained
Chronic pain syndrome is a complex condition that manifests as persistent pain lasting longer than six months. Unlike acute pain, which serves as a warning sign for injury, chronic pain often has no clear cause and can be difficult to manage.
This syndrome can result from various factors, including previous injuries, nerve damage, or conditions such as arthritis. Patients may experience pain that varies in intensity and can feel like a continuous ache, sharp jabbing, or burning sensation.
In addition to pain, chronic pain syndrome can lead to other symptoms, including fatigue, sleep disturbances, and emotional issues like depression or anxiety. These symptoms can significantly interfere with daily activities, making it harder for individuals to engage in work and personal relationships.
Treatment for chronic pain syndrome is often multi-faceted, combining medications, physical therapy, and psychological support. Management strategies may include lifestyle changes, relaxation techniques, and alternative therapies, aiming to improve quality of life for those affected.
Understanding sensory impairment
Sensory impairment refers to a reduction or loss of one or more senses, which may include vision, hearing, taste, touch, or smell. It can significantly affect daily activities and quality of life.
This type of impairment can arise from various causes, such as age-related degeneration, injuries, illnesses, or genetic conditions. For example, conditions like macular degeneration can lead to vision loss, while hearing loss can result from prolonged exposure to loud noises.
Individuals with sensory impairment often face challenges in communication, mobility, and social interaction. For instance, those with hearing impairments may struggle to engage in conversations, which can lead to feelings of isolation.
To accommodate sensory impairments, various strategies can be employed. Assistive devices, such as hearing aids or magnifiers, can enhance sensory functions. Additionally, creating environments that are accessible and supportive can greatly improve the well-being of those affected.
Understanding the nature of sensory impairment is fundamental in fostering empathy and providing appropriate support, allowing for better inclusion in all aspects of life.
Role of neuroinflammation in nerve health
The role of neuroinflammation in nerve health is crucial for understanding how the nervous system responds to injury and disease. Neuroinflammation occurs when immune cells in the nervous system, such as microglia, become activated in response to harmful stimuli.
While neuroinflammation is a protective mechanism, it can also become detrimental if it is excessive or prolonged. Chronic neuroinflammation may lead to nerve damage, resulting in various conditions such as neuropathic pain, multiple sclerosis, and even Alzheimer’s disease.
In cases of nerve injury, neuroinflammation can facilitate healing by clearing debris and supporting nerve regeneration. However, if the inflammatory response is not properly regulated, it can contribute to further deterioration of nerve function.
Understanding the dual nature of neuroinflammation is vital for developing treatments aimed at protecting nerve health. Researchers are exploring therapies that can balance the inflammatory response, promoting healing while preventing damage.
Ongoing studies are essential to comprehend the full impact of neuroinflammation on peripheral and central nervous systems, which could lead to targeted interventions for various neurological diseases.
Signs of myelin sheath damage
The myelin sheath is a protective layer surrounding nerve fibers, crucial for efficient nerve signal transmission. When this sheath is damaged, it can lead to various symptoms affecting the body’s functionality.
Common signs of myelin sheath damage include:
- Numbness or tingling in the limbs, which often indicates that nerve signals are not being properly transmitted.
- Muscle weakness or difficulty moving certain parts of the body, resulting in decreased coordination.
- Problems with balance, which can lead to increased risk of falls and injuries.
- Vision issues, such as blurred or double vision, may occur if the damage affects the nerves connecting to the eyes.
- Pain or discomfort, often felt as sharp shooting pains or chronic aching in the affected areas.
Individuals experiencing these symptoms should seek medical evaluation. Detecting myelin sheath damage early can lead to better management and treatment options, including medications and rehabilitation therapies.
Exploring autonomic dysfunction
Autonomic dysfunction refers to a condition where the autonomic nervous system (ANS) does not work properly. The ANS controls involuntary body functions, such as heart rate, digestion, and respiratory rate.
When this system is dysfunctional, it can lead to a range of symptoms, including:
- Heart rate abnormalities such as tachycardia (rapid heartbeat) or bradycardia (slow heartbeat), making it challenging for the body to respond to physical demands.
- Dizziness or fainting, especially when standing up quickly, due to improper blood flow regulation.
- Digestive problems, including constipation or diarrhea, stemming from irregular gastrointestinal motility.
- Temperature regulation issues, such as excessive sweating or feeling too hot or cold, because the ANS plays a key role in skin blood flow.
- Fatigue and difficulty concentrating, which can affect daily activities and overall well-being.
Conditions like diabetes, Parkinson’s disease, and multiple sclerosis can lead to autonomic dysfunction. Early diagnosis and treatment are crucial in managing symptoms and improving quality of life.
Effective treatments for neuropathy
Effective treatments for neuropathy depend on the underlying cause of the condition, as neuropathy can result from various factors such as diabetes, infections, or injuries. Here are some common treatment options:
Medications play a key role in managing neuropathy symptoms. Over-the-counter pain relievers like ibuprofen and naproxen can help reduce mild pain. For more severe symptoms, doctors may prescribe medications such as gabapentin or pregabalin, which target nerve pain specifically.
Physical therapy can also be beneficial. A physical therapist can design an exercise program to improve strength, flexibility, and coordination. This can help patients regain functionality and reduce discomfort.
Alternative therapies, such as acupuncture, have been reported to relieve pain and enhance nerve function. Some patients find relief through hot or cold therapies, which can soothe symptoms temporarily.
Dietary changes are significant as well. Maintaining healthy blood sugar levels through a balanced diet can help manage diabetic neuropathy. Foods rich in vitamins B1, B6, and B12 are particularly beneficial for nerve health.
Finally, addressing lifestyle factors such as quitting smoking and limiting alcohol can further support treatment efforts and promote overall nerve health.
Lifestyle changes to manage symptoms
Making lifestyle changes can significantly help manage symptoms of neuropathy and improve overall health. Here are some effective changes to consider:
1. Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can provide essential nutrients for nerve health. Foods high in omega-3 fatty acids, like salmon, are particularly beneficial.
2. Regular Exercise: Engaging in regular physical activity helps improve blood circulation, reduces pain, and supports nerve function. Activities like walking, swimming, and yoga can be especially helpful.
3. Stress Management: Chronic stress can worsen symptoms of neuropathy. Practices such as meditation, deep breathing exercises, or tai chi can help reduce stress levels.
4. Quit Smoking: Smoking can constrict blood vessels and decrease blood flow to the nerves, worsening symptoms. Quitting smoking is essential for improving nerve health.
5. Limit Alcohol: Excessive alcohol consumption can lead to further nerve damage. It is advisable to limit or eliminate alcohol for better symptom management.
6. Manage Blood Sugar: For those with diabetic neuropathy, keeping blood sugar levels stable is critical. Regular monitoring and adherence to treatment plans can help prevent future complications.
Making and maintaining these lifestyle changes can greatly enhance quality of life and reduce the impact of neuropathy symptoms.
Managing Neuropathy: A Holistic Approach
Managing neuropathy requires understanding its causes, symptoms, and effective treatments. With the right lifestyle changes, individuals can significantly improve their quality of life.
By focusing on a balanced diet, regular exercise, and stress management techniques, you can help alleviate symptoms and support overall nerve health. Additionally, seeking appropriate medical treatment and maintaining regular check-ups will play a crucial role in your management plan.
Remember, with patience and a proactive approach, you can take charge of your health and find relief from the challenges of neuropathy.
FAQ – Frequently Asked Questions about Neuropathy Management
What are the common symptoms of neuropathy?
Common symptoms include numbness, tingling, sharp pain, muscle weakness, and difficulty walking.
How can lifestyle changes help manage neuropathy symptoms?
Lifestyle changes such as maintaining a healthy diet, regular exercise, stress management, and avoiding alcohol can significantly improve symptoms.
What dietary supplements are beneficial for nerve health?
Vitamins B1, B6, and B12 are particularly beneficial for nerve health, along with omega-3 fatty acids found in fatty fish.
What are the effective treatments for neuropathy?
Effective treatments may include medications, physical therapy, alternative therapies like acupuncture, and lifestyle adjustments.
How important is blood sugar control for diabetic neuropathy?
Maintaining stable blood sugar levels is crucial for managing diabetic neuropathy and preventing further nerve damage.
When should I see a doctor about my neuropathy symptoms?
You should see a doctor if your symptoms worsen, interfere with daily activities, or if you experience new symptoms.

Max is a health and wellness researcher dedicated to optimizing human performance through science-backed protocols. As a contributor to High Performance Protocols, he analyzes the latest medical studies and translates complex research into practical, easy-to-follow strategies for improving energy, longevity, and overall well-being. Passionate about biohacking, nutrition, and evidence-based health solutions, Max Reynolds helps readers navigate the ever-evolving world of health optimization with clarity and precision.