Neuropathy, classified in ICD 10, affects the peripheral nervous system and can manifest through symptoms like tingling, numbness, and pain, while effective management includes medications, lifestyle modifications, and dietary changes.
Neuropathy nos ICD 10 is more than just a diagnosis; it affects daily lives in subtle yet challenging ways. Are you curious about how it impacts you or your loved ones? Let’s delve into what this means for effective management and relief.
What is neuropathy and its significance in ICD 10?
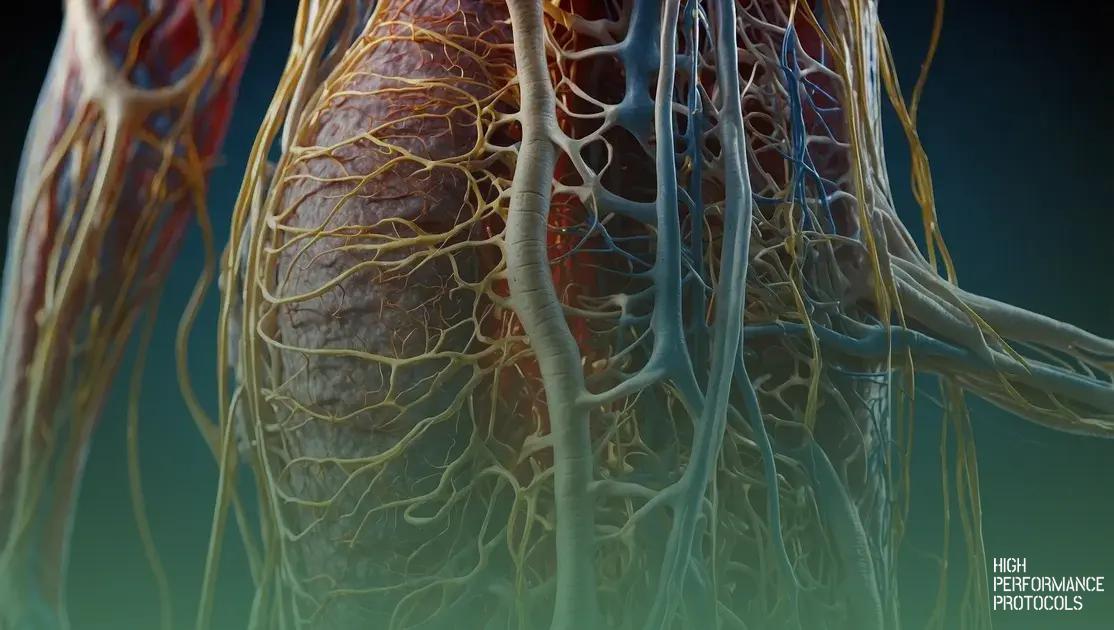
Neuropathy is a condition that affects the peripheral nervous system, leading to various symptoms such as pain, tingling, or weakness. In the ICD 10 (International Classification of Diseases, 10th Revision), neuropathy is classified under different codes based on its specific type and cause. Understanding these classifications is crucial for proper diagnosis and treatment.
There are several types of neuropathy described in the ICD 10, including diabetic neuropathy, which often arises due to prolonged high blood sugar levels. Each type of neuropathy has its distinct symptoms and requires tailored management strategies.
Significance of ICD 10 Classifications
The significance of these classifications lies in their ability to help healthcare providers accurately diagnose and treat patients. By referencing specific ICD 10 codes, doctors can communicate about the condition effectively and ensure that patients receive appropriate care. Moreover, these codes facilitate research and public health reporting, enhancing our understanding of how neuropathy affects populations.
Awareness of the different classifications can empower patients as well. When individuals understand their diagnosis better, they can engage more actively in discussions about their treatment options and advocate for their health.
Understanding symptoms of neuropathy
Neuropathy can manifest through various symptoms that affect how individuals function in their daily lives. Some common symptoms include:
- Tingling Sensation: Many people experience a prickly or tingling feeling in their hands and feet, often referred to as “pins and needles.” This sensation can be intermittent or persistent.
- Numbness: Loss of feeling in the affected areas is frequent, making it difficult for individuals to sense temperature changes or pain.
- Weakness: Muscle weakness is prevalent, particularly in the legs and arms, which can hinder mobility and daily activities.
- Burning Pain: Some may feel a burning sensation that can be quite uncomfortable, impacting sleep or relaxation.
- Sensitivity: Increased sensitivity to touch, known as allodynia, can occur, where even light touch may cause pain.
Recognizing these symptoms early is essential for seeking appropriate treatment and care. If you or someone you know is experiencing these issues, consulting a healthcare professional is recommended.
Types of neuropathy classified in ICD 10
The ICD 10 classifies neuropathy into various types, each with specific codes that help healthcare professionals diagnose and treat these conditions effectively. Here are some of the main types of neuropathy found in the ICD 10:
- Diabetic Neuropathy (E11.4): This occurs due to long-term high blood sugar levels, affecting nerves, particularly in the legs and feet.
- Peripheral Neuropathy (G62.9): This generic term describes any disorder affecting the peripheral nerves, with numerous causes, including trauma and infections.
- Idiopathic Neuropathy (G62.9): This type has no known cause, making diagnosis and treatment more challenging.
- Alcoholic Neuropathy (G62.1): Chronic alcohol abuse can lead to nerve damage, specifically affecting the legs and feet.
- Hereditary Neuropathies (G60): These include genetic conditions that affect the nerves, resulting in various symptoms.
Each type of neuropathy requires specific treatment approaches and management plans. Understanding these classifications aids in recognizing symptoms and pursuing effective therapies.
Diagnosis: How is neuropathy identified?
The diagnosis of neuropathy involves a comprehensive approach to identifying the condition accurately. Healthcare providers typically use several methods to diagnose neuropathy effectively:
- Medical History: A detailed medical history is crucial. Doctors will ask about symptoms, their duration, and any previous illnesses or conditions that might contribute to nerve damage.
- Physical Examination: A thorough physical exam helps assess muscle strength, reflexes, and sensory responses. This examination can reveal areas of weakness or loss of feeling.
- Nerve Conduction Studies (NCS): This test measures how well electrical signals travel through a nerve. It helps determine the severity and type of nerve damage.
- Electromyography (EMG): EMG records the electrical activity of muscles. It can identify if the muscle weakness is due to nerve issues or conditions affecting the muscles themselves.
- Blood Tests: Blood tests help identify underlying conditions that might lead to neuropathy, such as diabetes, vitamin deficiencies, or autoimmune disorders.
- Imaging Tests: Imaging tests like MRI or CT scans can assess for other potential causes of nerve damage, such as tumors or structural abnormalities.
Combining these diagnostic methods allows doctors to form a clear picture of the patient’s condition, leading to effective treatment strategies.
Treatment options for managing neuropathy
Treatment for neuropathy varies based on the underlying cause and type of neuropathy. Here are several effective treatment options that healthcare providers may recommend:
- Medications: Pain relief medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), antidepressants, and anticonvulsants, can help manage symptoms. Capsaicin cream may also be used for localized pain relief.
- Physical Therapy: Physical therapy can help improve strength, coordination, and mobility. A therapist will create a personalized exercise program to enhance function and minimize discomfort.
- Occupational Therapy: Occupational therapy focuses on helping individuals adapt to their environment and perform daily tasks. Therapists may suggest adaptive devices to ease daily activities.
- Dietary Changes: Nutritional adjustments, including a balanced diet rich in vitamins (especially B vitamins) and minerals, can support nerve health. Supplementing with specific vitamins may also be beneficial, depending on individual needs.
- Alternative Therapies: Some patients find relief through acupuncture, chiropractic care, or massage therapy. These therapies can promote relaxation and may alleviate some neuropathy symptoms.
- Lifestyle Modifications: Quitting smoking, reducing alcohol consumption, and managing blood sugar levels (for diabetic neuropathy) are essential steps in slowing progression and managing symptoms.
It is crucial to consult with a healthcare provider to determine the most appropriate treatment plan tailored to individual needs and conditions.
Dietary changes to support nerve health
Making dietary changes can significantly support overall nerve health and help manage symptoms of neuropathy. Here are some important dietary tips to consider:
- Increase B Vitamins: Vitamins B1, B6, and B12 are essential for nerve function. Foods rich in these vitamins include whole grains, beans, nuts, seeds, fish, and lean meats.
- Eat Antioxidant-Rich Foods: Antioxidants help protect nerves from damage. Incorporate plenty of fruits and vegetables such as berries, spinach, broccoli, and bell peppers.
- Include Healthy Fats: Omega-3 fatty acids, found in fatty fish like salmon, walnuts, and flaxseeds, can promote nerve repair and overall brain health.
- Limit Sugar and Processed Foods: High sugar intake and processed foods can worsen nerve damage, especially in diabetic patients. Focus on whole, natural foods instead.
- Stay Hydrated: Proper hydration is crucial for maintaining nerve health. Drink plenty of water throughout the day to support bodily functions.
- Consider Anti-Inflammatory Foods: Turmeric, ginger, and green tea have anti-inflammatory properties that may benefit nerve health. Incorporate these into meals for added benefits.
Consulting a nutritionist or healthcare provider can personalize dietary recommendations based on individual health needs and conditions.
Lifestyle modifications to ease neuropathy symptoms
Making lifestyle modifications can significantly help in managing and easing the symptoms of neuropathy. Here are several effective changes to consider:
- Regular Exercise: Engaging in regular physical activity can improve blood flow, reduce pain, and enhance muscle strength. Simple activities like walking, swimming, or cycling are beneficial.
- Maintain a Healthy Weight: Keeping a healthy weight can alleviate pressure on nerves, particularly in the legs and feet. A balanced diet paired with regular exercise helps in weight management.
- Quit Smoking: Smoking can worsen circulation and contribute to nerve damage. Quitting smoking can significantly improve nerve health and overall well-being.
- Limit Alcohol Consumption: Excessive alcohol intake can lead to further nerve damage. Reducing alcohol consumption, or avoiding it altogether, may help in managing symptoms.
- Stress Management: High stress can exacerbate neuropathy symptoms. Practicing relaxation techniques such as deep breathing, yoga, or meditation can help reduce stress.
- Foot Care: Regularly check your feet for injuries or sores, especially if you have diabetic neuropathy. Keeping feet clean and well-moisturized can prevent complications.
Incorporating these lifestyle changes can empower individuals dealing with neuropathy to better manage their symptoms and improve their quality of life.
Finding support groups and resources for neuropathy
Finding support groups and resources for managing neuropathy can be beneficial for individuals coping with the condition. Here are some options to consider:
- Online Support Groups: Many websites and forums, such as the Neuropathy Association and the Foundation for Peripheral Neuropathy, offer online communities where individuals can share experiences, get advice, and find emotional support.
- Local Support Groups: Check with local hospitals, community centers, or health organizations for in-person support groups. Connecting with others in your area can provide valuable social support.
- Social Media Communities: Platforms like Facebook have numerous groups dedicated to neuropathy where members share tips, resources, and uplifting stories to foster a sense of belonging and encouragement.
- Educational Resources: Organizations such as the American Academy of Neurology provide comprehensive information dealing with various types of neuropathy, treatment options, and management strategies. These resources can help you stay informed about your condition.
- Healthcare Providers: Don’t hesitate to ask your doctor or neurologist for recommendations on support groups and resources. They may know local or online options that can help.
Using these resources can empower individuals with neuropathy, providing them with the knowledge and support they need for effective management.
Managing Neuropathy: A Path to Better Health
Living with neuropathy can be challenging, but understanding the condition is the first step towards effective management. By recognizing symptoms and exploring treatment options, individuals can take control of their health.
Adopting lifestyle changes, making dietary adjustments, and seeking support through groups and resources can significantly improve quality of life. Remember, every small step counts, and connecting with others facing similar challenges can provide not only information but also comfort.
With the right knowledge and support, managing neuropathy can lead to a healthier, more fulfilling life.

Max is a health and wellness researcher dedicated to optimizing human performance through science-backed protocols. As a contributor to High Performance Protocols, he analyzes the latest medical studies and translates complex research into practical, easy-to-follow strategies for improving energy, longevity, and overall well-being. Passionate about biohacking, nutrition, and evidence-based health solutions, Max Reynolds helps readers navigate the ever-evolving world of health optimization with clarity and precision.